Maintaining oral hygiene while wearing braces is crucial for a healthy smile and preventing future dental issues. One common question that arises among individuals with braces is whether they can use an electric toothbrush. Well, using an electric toothbrush with braces can be tricky, and whether using it is a good idea is something people with braces should know. Let’s delve deep in and explore the benefits and considerations of using an electric toothbrush with braces while learning proper toothbrushing techniques.
Understanding Everything About Electric Toothbrushes
Electric toothbrushes are powered or run by a battery or electricity and come with various features such as oscillating, rotating, or vibrating brush heads. These features help improve the cleaning process by effectively removing plaque and food particles from the teeth and gums.
What are the Benefits of Using an Electric Toothbrush With Braces
There are various benefits of using an electric toothbrush with braces. Electric toothbrushes are completely safe to use with braces and give good oral hygiene results when used properly. Below are some of these benefits you should know about:
- Efficient Cleaning: Electric toothbrushes can reach difficult-to-access areas around braces. This ensures a thorough cleaning of the teeth and brackets.
- Gentle on Braces: Many electric toothbrushes come with sensitive mode settings, which make them gentle on braces and reduce the risk of damaging wires or brackets.
- Timer and Pressure Sensors: Some models have built-in timers and pressure sensors that alert users when brushing too hard or when they need to move to a different area. This promotes proper toothbrushing techniques and good oral hygiene.
- Consistent Brushing: The consistent motion of electric toothbrushes helps maintain a consistent brushing technique, which is essential for effective plaque removal.
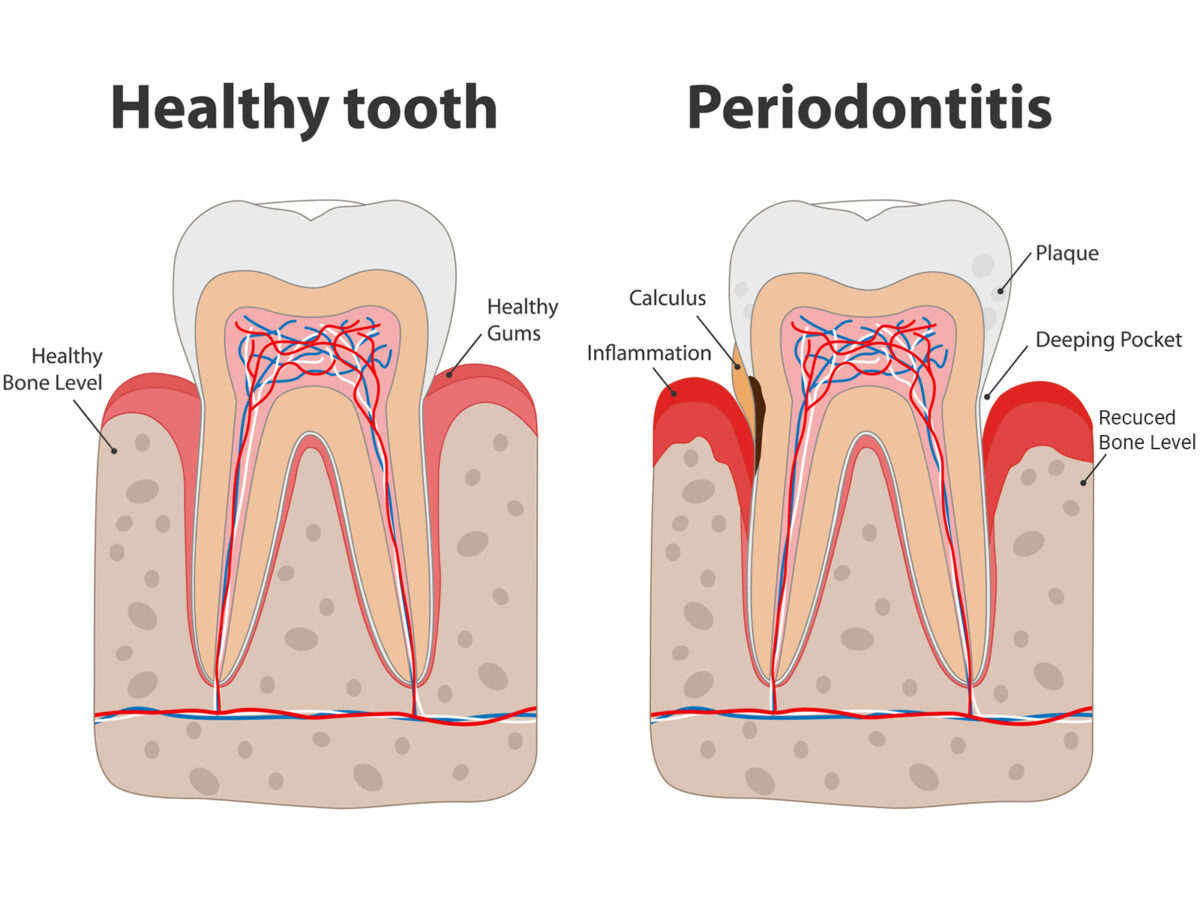
- Improved Gum Health: Proper oral hygiene with an electric toothbrush can contribute to healthier gums, reducing the risk of gum disease during orthodontic treatment.
Some Considerations When Using an Electric Toothbrush With Braces
Here are some considerations that you should keep in mind while using an electric toothbrush with braces:
Brush Head Compatibility: Ensure the electric toothbrush you choose has a brush head suitable for braces. Look for brush heads specifically designed for orthodontic patients.
Brushing Technique: Make sure to follow the recommended toothbrushing techniques provided by your orthodontist or dentist. Angle the brush head to clean around brackets and wires gently.
Regular Maintenance: You should clean and replace the brush head regularly to maintain optimal cleanliness and effectiveness.
Consult Your Orthodontist: Before using an electric toothbrush with braces, consult your orthodontist for personalized advice and recommendations based on your specific orthodontic treatment.
Tips for Effective Toothbrushing With Braces
Here are some tips for effective toothbrushing with braces:
- Use Fluoride Toothpaste: Choose a fluoride toothpaste to help strengthen tooth enamel and prevent tooth decay, especially around brackets.
- Floss Daily: Include flossing into your daily oral hygiene routine to remove plaque and food debris from between teeth and braces.
- Attend Regular Check-ups: Schedule regular dental check-ups with Rockdale Dentist TX to monitor your oral health and address any issues promptly.
- Stay Hydrated: Drink plenty of water to help flush away food particles and bacteria, reducing the risk of plaque buildup.
Conclusion
In conclusion, using an electric toothbrush with braces can be beneficial for maintaining optimal oral hygiene during orthodontic treatment. However, it’s important to choose the right brush head, follow recommended brushing techniques, and consult your orthodontist for personalized guidance. By combining proper toothbrushing techniques and regular dental care, you can ensure a healthy smile throughout your orthodontic journey.